The Cognitive Sanctuary: A 3-Step Ritual to Reclaim Clarity During Perimenopause & Menopause
By NovaPause Editorial Collective
Have your thoughts begun to feel less precise lately?
You walk into a room and pause. A familiar word hovers just out of reach. A task you have done many times suddenly requires more effort than expected.
Brain fog during perimenopause and menopause is common. It is not a loss of intelligence. It is not decline.
It reflects neurological and metabolic recalibration.
Clarity is not disappearing. The brain is adapting to hormonal change.
In this article, we explore what is happening physiologically and how to support cognitive steadiness during this stage. The focus is not on forcing productivity, but on creating the conditions that allow mental clarity to reemerge more consistently.
If you’d like the broader hormonal framework behind these changes, see:
• Perimenopause 101
• Managing Symptoms
• Brain Fog
Why Brain Fog Happens in Perimenopause & Menopause
Cognitive symptoms in midlife are closely tied to shifts in estrogen, metabolism, and nervous system regulation.
1. Changes in Brain Energy Use
Estrogen plays an important role beyond reproduction. It helps support how brain cells use glucose, maintain communication between neurons, and regulate mood and focus.
As estrogen fluctuates and later declines, the brain adjusts how it sources and uses energy. During this transition, some women notice:
Slower recall
Word finding difficulty
Mental fatigue
A sense of fuzzy or static focus
Research increasingly describes this period as transitional remodeling. The brain remains capable of adaptation.
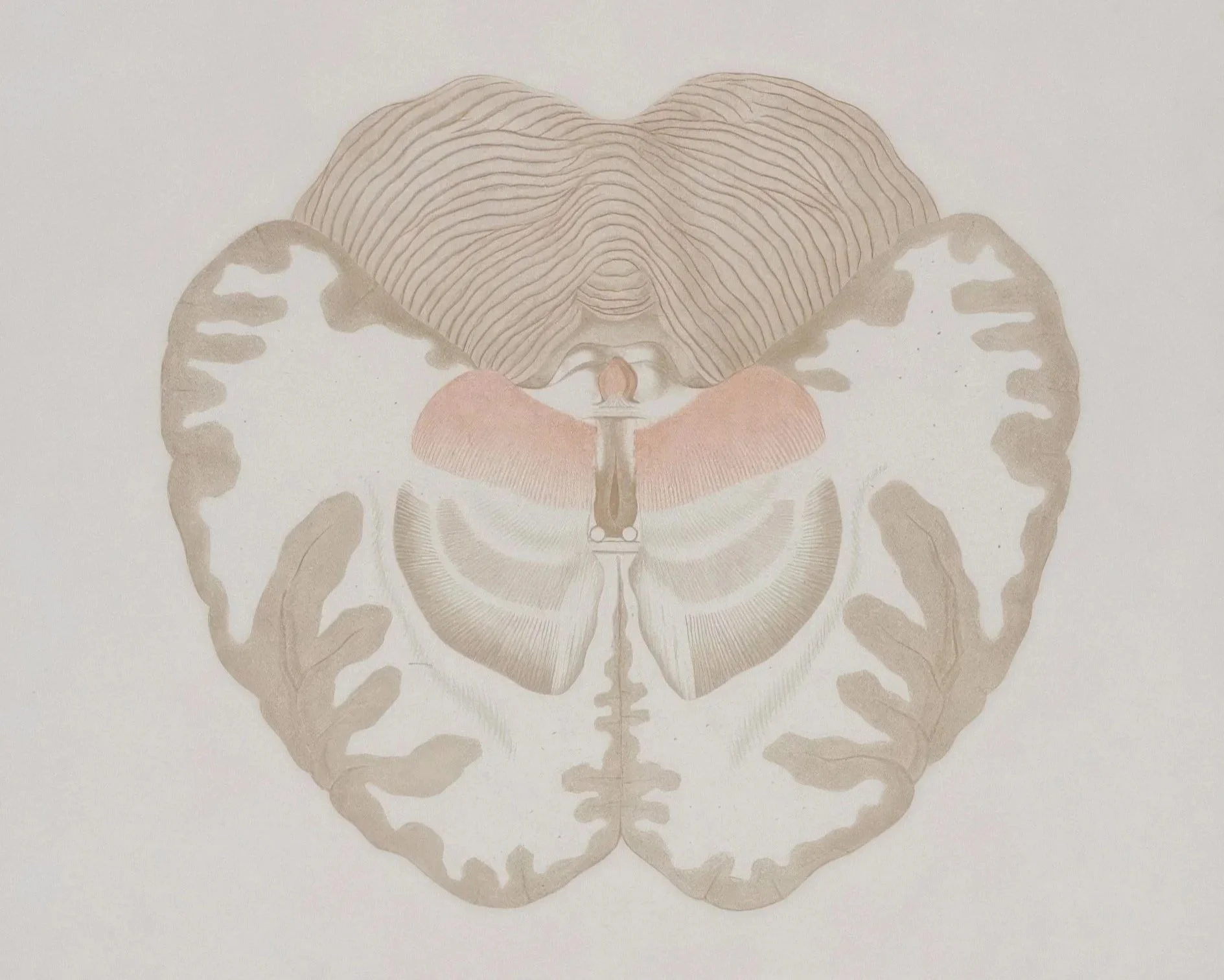
2. Neurological Remodeling
The menopausal transition involves measurable changes in neural connectivity. Researchers describe this as remodeling rather than degeneration.
Short term, this can feel disruptive. Long term, many women report:
Stronger pattern recognition
Greater emotional regulation
Clearer prioritization
A deeper sense of discernment
For more context on metabolic shifts that intersect with cognition, see: Midlife Metabolism: Reframing Weight in Menopause.
The Cognitive Sanctuary Ritual: A 3-Step Path Toward Clarity
This ritual is not about productivity or optimization. It is about supporting the brain through nourishment, nervous system regulation, and restorative rest.
You can begin with one step and build gradually.
Step 1: Support the Brain with Steady Fuel
The brain consumes a significant share of daily energy. During perimenopause and menopause, blood sugar variability can amplify cognitive symptoms.
1. Morning Hydration Anchor
After sleep, mild dehydration is common.
You might experiment with a simple morning ritual, such as:
A glass of room-temperature water
Optional addition of citrus and mineral salt if aligned with your health plan
This supports circulation and cellular function. It is not a treatment, but it establishes metabolic steadiness.
2. Balanced Meals for Cognitive Stability
Clarity is sensitive to blood sugar variability. A stabilizing, brain-supportive plate often includes:
Protein to help support steady energy and neurotransmitter production
Fiber-rich carbohydrates (vegetables, fruit, whole grains, legumes) for gradual blood sugar curves
Healthy fats to support cell membranes and satiety
Examples you might try:
Greek yogurt or cottage cheese with berries, ground flax, and walnuts
Eggs with sautéed greens and avocado
A tofu scramble with vegetables and olive oil
The goal is not restriction. It is steadiness.
For foundational nutrition structure, see: Balancing Hormones on Your Plate.
3. Omega-3 and Brain Lipids
Omega-3 fatty acids (EPA and DHA) are studied for their role in neuronal membrane health and inflammation modulation. Food sources include salmon, sardines, walnuts, chia, flax.
For women exploring supplementation, one third-party-tested formulation aligned with cognitive research standards is: Thorne Memoractiv.
For women exploring botanical and nootropic blends formulated for midlife cognition: OPositive Meno Capsules.
If you’re considering new supplements or oils, it’s always wise to check in with a healthcare provider, especially if you have a history of digestive, metabolic, or cardiovascular conditions.
These are optional tools within a broader nutritional framework, not primary interventions.
Step 2: Regulate Nervous System Load
Hormonal shifts can heighten sympathetic activation. When stress is amplified, focus becomes harder to access.
Clarity requires nervous system steadiness.
1. 1-Minute Breath Reset
When your mind feels scattered, try pausing for a short, structured breath practice:
1-Minute 4–4–6 Breath
Inhale gently for a count of 4
Hold that breath for a comfortable count of 4
Exhale slowly for a count of 6
Repeating this for one to three minutes can support parasympathetic activity and improve focus.
2. Light Cognitive Engagement
On lower-clarity days, intense focus can feel counterproductive.
Instead try one of these:
Creative hobbies
Language exposure
Music
Gardening
Hands on tasks
These gently stimulate neuroplasticity without overload.
3. Intentional Pauses
When the fog rolls in:
Step away from the screen or task, even for a minute
Take a few slow breaths
Do a quick stretch, sip water, or look out a window
This respects the reality that the brain may need more frequent recovery during this phase.
Guided Regulation Tools (Optional)
For women who prefer structured cues, devices designed for nervous system support include:
These devices are designed to provide external cues that support nervous system down-regulation. They are not required but may complement foundational practices.
For a broader integrative framework, see: Holistic Wellness.
Step 3: Protect Restorative Sleep
Sleep is where your brain has a chance to reset, consolidate memories, and clear metabolic byproducts. When sleep is fragmented, as it often is in perimenopause and menopause, brain fog can intensify.
For a deeper dive, see our post on Reclaiming Your Nights: A Sleep Sanctuary Plan for Perimenopause.
1. Cool, Breathable, and Dark
Many women find they sleep better when their bedroom is:
Slightly cool
As dark as realistically possible
Breathable bedding
Layered blankets
A sheet set aligned with moisture regulation principles: Cozy Earth Bamboo Sheets.
The goal isn’t to eliminate every hot flash, but to create an environment that makes temperature swings less disruptive.
2. Create a “Digital Sunset”
Reduce blue light exposure 30–60 minutes before bed.
Replace scrolling with:
Stretching
Light reading
Warm shower
Breath practice
3. Evening Nutritional Support
Some women also incorporate an evening magnesium drink such as Moon Juice Neuro MagnesiOm or calming herbal tea like Rishi Chamomile Medley as part of this wind-down.
Magnesium and herbal teas may support relaxation. They are supportive rituals, not sedatives.
Always consult a healthcare provider before starting supplements.
4. Explore Non-Sleep Deep Rest (NSDR) or Yoga Nidra
On nights when sleep feels elusive, structured rest practices can provide meaningful nervous system recovery.
Non-Sleep Deep Rest (NSDR) and Yoga Nidra are guided protocols designed to support parasympathetic activation without requiring traditional meditation.
Typically, you:
Lie down in a comfortable position
Listen to an audio track that leads you through body scanning, relaxation, or breath awareness
These practices are not a replacement for sleep, but many women find they:
Ease mental tension
Support emotional calm
Reduce next-day fatigue
Sometimes make it easier to drift into sleep afterward
Even 10–20 minutes can feel surprisingly restoring.
For women navigating menopause-related brain fog, this type of intentional rest can be a powerful bridge between exhaustion and recovery.
Clarity Changes with Care
Cognitive clarity tends to return gradually.
Often in subtle ways:
More consistent focus windows
Easier word retrieval
Less frustration when fog appears
A steadier internal pace
Mental sharpness in midlife often becomes less frantic and more deliberate.
The brain reorganizes. It does not disappear.
Why Tracking Matters
Patterns are more informative than isolated symptoms.
Use the link below to go to our sign-up page, enter your email, and we’ll send the tracker straight to your inbox. Over one week, tracking may include:
When brain fog appears
How sleep and temperature changes relate to clarity
Which habits seem to support focus
✨ Get the free 7-Day Symptom & Pattern Tracker.
Clarity is not a fantasy. It is often a function of alignment.
Affiliate Disclosure
NovaPause participates in affiliate programs, including the Amazon Services LLC Associates Program. This means NovaPause may earn a commission from qualifying purchases made through links on this site, at no additional cost to you.
Important Medical Disclaimer:
This article is for educational purposes only and is not intended to diagnose, treat, cure, or prevent any disease. Always consult with your healthcare provider about your specific symptoms, medical history, and before starting or changing any supplement, medication, or wellness practice.